Indigestion is also commonly referred to as dyspepsia or upset stomach and it is the burning or painful feeling that is felt on the upper part of the abdomen. Indigestion is not necessarily a diverse condition, but it might be a symptom of an intestinal problem like gallbladder disease, peptic ulcers or also chronic appendicitis. Indigestion can be caused or occurs when acid in the stomach flows back up the oesophagus. The oesophagus is the pipe that connects the mouth to the stomach. This problem can also occur when the stomach is inflamed of irritated. Many people have suffered from indigestion after indulging in a large meal at some point. Additionally, most people suffer from heartburn every year. Indigestion can occur at any time even though it is most commonly experienced after meals.
There are several elements that may cause indigestion. Moreover, to establish that one is suffering from indigestion, the person needs to identify the symptoms that are associated with the problem. The symptoms may range from heartburn to loss of appetite, to flatulence, the passing of gas from the rectum, to belching or burping, from feeling sick to fullness, pain or discomfort in the upper part of the abdomen or chest. The symptoms vary depending on what one is suffering from. Depending on the disease that one is suffering, which is the source of the condition, the symptoms may dissipate very quickly, almost immediately, come and go, or could last for a long period of time. Indigestion is caused by the strong acid that is produced in the stomach, which assists in the digestion of food and protects the stomach against infections. There is a layer of mucous on the stomach lining, which acts as a barrier against the acid and if this mucous layer is damaged, the tissues that are found underneath this layer can be irritated by the acid.
Some of the following items can trigger the above symptoms and thus cause the condition. Excessive consumption of alcohol, stress and anxiety, smoking, medicinal drugs like anti-inflammatory medicines that are utilized for treating arthritis and aspirin. Also, the consumption of certain food types can cause the sphincter or valve to relax, where the stomach and oesophagus link or cause direct irritation to the oesophagus lining and this causes indigestion. Additionally, skipping or missing one’s regular meals could cause acid levels to build up. There are other major causes of indigestion like heartburns, peptic ulcers, cancer, pregnancy and many other complications.
Do You Have GERD?
Have you ever had heartburn? You know, that feeling of discomfort, nausea, and “indigestion” in your stomach? Maybe it only happens once in a while, or maybe it happens on a daily basis.
Either way, dealing with heartburn can be uncomfortable and unpleasant. Depending on when it happens, it can affect your appetite, your sleep, and your health in general. If it’s happening regularly, you may have something called gastroesophageal reflux disease (GERD).
GERD is basically a chronic form of acid reflux, and it affects roughly 20% of Americans.¹
While there are many things that can increase the risk of having GERD, it really comes down to a certain part of the stomach not working properly. This allows the leakage or “reflux” of stomach contents into the esophagus (the tube that connects the mouth to the stomach).
If you think that you may have GERD but you’re not sure where to begin, you’ve come to the right place.
What is Acid Reflux?
GERD is a condition that happens as a result of stomach contents leaking out of the stomach and into something called the esophagus. The esophagus is a long tube that connects the mouth to the stomach.
There is something called the lower esophageal sphincter, which lies in between the esophagus and the stomach. The job of this sphincter is to prevent stomach contents from leaking out into the esophagus. However, when this sphincter doesn’t work properly, stomach contents can move back into the esophagus. You can see this in the image below:
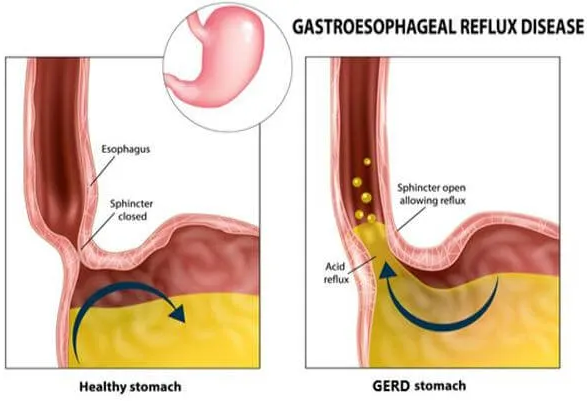
When the “reflux” of stomach contents happens, it can cause unpleasant symptoms. This is because our stomach contents contain different acids that help our body break down and digest the food we eat. But when it leaks out into the esophagus, it can result in inflammation and irritation.
The severity of the inflammation caused by acid reflux can vary, and this is why GERD is broken down into three types:³
- Non-erosive reflux disease: This type of acid reflux can cause some mild inflammation of the stomach and esophagus, but it doesn’t cause any erosion or breakdown. This is the most common type of acid reflux, and it makes up about 60–70% of cases of GERD.
- Erosive esophagitis: As you can probably tell with the name, this type of acid reflux involves the inflammation and breakdown of the lining of the esophagus. It accounts for about 30% of cases of GERD.
- Barrett’s esophagus: This last type of acid reflux is the most uncommon and only makes up about 6–12% of cases. It causes the end of the esophagus near the sphincter to become thickened and red. These changes that happen are a result of severe inflammation caused by untreated GERD. And unfortunately, this type of GERD is associated with an increased risk of cancer of the esophagus.⁴
It’s important to note that there are certain cells in the lining of the stomach that produce the acids our bodies need to digest food. The main cells are called parietal cells. This understanding will come into play when we discuss how acid reflux is treated.
But first, we should understand what causes GERD.
What Causes Acid Reflux?
At the moment, there isn’t any one thing in particular that causes GERD. But based on how GERD works, research has been able to find certain risk factors for developing GERD.
Certain medical conditions have an impact on the structure and motility of the stomach and esophagus, which can result in the development of GERD. Having these conditions can increase the risk of developing GERD:³
- Esophageal dysmotility
- Delayed gastric emptying (gastroparesis)
Another common risk factor for developing GERD is obesity. This is because carrying excess weight around the stomach increases pressure within the abdominal cavity. This increased pressure can cause stomach contents to move out of the stomach and into the esophagus.
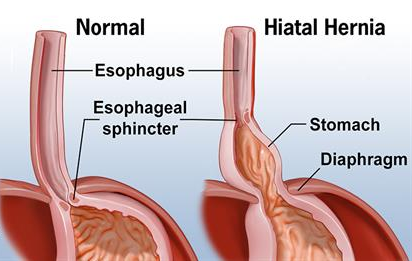
And as you can see in the image below, having a hiatal hernia can cause the same thing.
The significance of GERD and obesity has been studied a lot, and it’s been found that in people with both obesity and GERD, the risk of developing erosive esophagitis increases with weight.⁶
Other risk factors for developing GERD include:
- Being over the age of 50 years
- Tobacco use
- Drinking a lot of alcohol
- Pregnancy
- Lying down on your back after eating
Types of medications that have been shown to increase the risk of GERD include:³
- Anticholinergic drugs, like Benadryl and Dramamine
- Benzodiazepines, like Ativan and Xanax
- Non-steroidal anti-inflammatory drugs (NSAIDs), like Aleve, Ibuprofen, Motrin, and Aspirin
- Nitroglycerin
- Albuterol
- Calcium channel blockers, like Cardizem
- Tricyclic antidepressants, like Amitriptyline
- Glucagon
Now that you know what GERD is and what can increase the risk of having it, how do you know if you have it?
What Are the Symptoms of Acid Reflux?
The symptoms of GERD are caused by irritation and inflammation of the esophagus. Depending on the severity of the inflammation, some of the symptoms can be so severe that they mimic conditions like heart attacks.
Common symptoms of GERD include:⁷
- Indigestion
- Nausea
- Bloating
- Sore throat
- The feeling of a lump in your throat
- Upper abdominal pain
These symptoms will often worsen when lying flat, especially after a meal. This is because lying flat makes it easier for stomach acid to move up into the esophagus.
Some less frequent symptoms of GERD can include chest pain and chronic cough. There are even cases when uncontrolled GERD can cause asthma, sinusitis (inflammation of the sinuses), dental erosions (breakdown of the teeth), and recurrent otitis media (inner ear infections).⁷
It’s important to note that even if you have GERD and you develop new chest pain, you shouldn’t just blame it on the GERD. It’s still important to get any new chest pain evaluated in an emergency department because it could be due to a heart attack.
How Is Acid Reflux Diagnosed?
GERD is typically a clinical diagnosis. This means that your healthcare provider will ask you certain questions and perform a physical exam. If you have the signs and symptoms of GERD, it can be diagnosed. Typically, treatment with lifestyle changes and medications is started. But if things aren’t getting better, further testing may be needed.
Sometimes, GERD is diagnosed with testing called an endoscopy (EGD). An EGD is a procedure where you’re put to sleep and a small camera is passed into your stomach and the first part of your small intestine. This procedure only takes about 15 minutes, and a lot of information can be gathered. This includes the ability to take a direct look into your esophagus and stomach as well as the ability to get biopsies.
Getting a biopsy done during an EGD is standard procedure and allows doctors to check for other causes of GERD such as:
- Helicobacter pylori: A bacterial infection that can cause inflammation and ulcers in the stomach.
- Eosinophilic esophagitis: An allergic/immune system condition where certain white blood cells called eosinophils accumulate in the esophagus. This causes inflammation of the esophagus and can result in symptoms that are similar to GERD.
If your EGD is normal and you’re not getting better with treatment, some providers will try something called an ambulatory esophageal pH monitor. It’s a device that is temporarily placed into the base of the esophagus to monitor how bad the reflux of stomach contents is. Here is a video that explains it a bit more:
It’s important to note that there are certain signs and symptoms that may require you to have an EGD sooner. These symptoms include:⁸
- Difficulty swallowing
- Painful swallowing
- Blood in your stool, which can present like bright red stool or dark red/black stool
- Weight loss
- Getting full quickly
These symptoms can be a sign of serious conditions like cancer and bleeding in the stomach or intestines. If you have blood in your stool of any kind, it’s recommended that you present to the nearest emergency department as soon as possible. Blood in the stool can be life-threatening. The other symptoms listed above, while serious, don’t often require emergent evaluation in a hospital.
How Is Acid Reflux Treated?
Once your GERD has been diagnosed, either clinically or by a test such as an EGD or esophageal pH monitor, your healthcare provider will recommend different treatments to help improve your condition.
A lot of research has been done into the different treatments for GERD, and many lifestyle modifications, especially weight loss, has been found to be effective for many people. There are also several different medications that are FDA-approved for the treatment of GERD.
